7 Balance Exercises Seniors Can Do Every Day
Table of contents
Mastering proper gait exercises can significantly enhance the balance ability of the elderly.
Visual focus control and action rhythm have a significant impact on walking stability.
Implementing progressive balance training programs in daily home environments.
Single-leg standing training requires appropriate support and safety measures.
Hip strengthening exercises play a key role in fall prevention.
Key practices for enhancing functional strength through chair stand training.
The organic integration of traditional health exercises and modern rehabilitation concepts.
1. Heel-to-Toe Walking Technique
Action Principles and Effectiveness Analysis
This gait training activates the lower limb proprioceptor network by precisely controlling the foot contact surface. When the heel and toe form a continuous contact line, the muscle groups around the ankle joint will undergo slight dynamic adjustments, and this continuous adjustment mechanism is key to enhancing balance ability. It is worth noting that data from the American College of Sports Medicine shows that continuous training of this type can reduce the probability of accidental falls in the over 65 age group by 28-34%.
During training, special attention should be paid to the choice of environment. It is recommended to initially practice in a corridor with anti-slip mats, using the wall as auxiliary support. As ability improves, practicing on a soft carpet can further enhance neuromuscular control through ground feedback differences.
Phase-Based Training Program Design
Beginners can adopt a three-steps-and-a-stop approach: pause for 2 seconds to adjust the center of gravity after completing three heel-to-toe contacts. Intermediate practitioners can try walking while holding a cup with gradually decreasing water volume, adding both challenge and fun. It is particularly important to keep the gaze horizontal; looking down too much can cause the center of gravity to shift forward and lead to imbalance.
Common Pitfalls and Improvement Strategies
Most practitioners are prone to speed anxiety and hastily increase step frequency, which undermines the training effect. It is recommended to use a metronome, initially setting the rhythm to 60 beats per minute and increasing by 5 beats every two weeks. Another common issue is stiff arms; holding a lightweight stick (of shoulder width) during practice can help promote natural swinging and coordinate the entire body's mechanical chain.
2. Single-Leg Support Balance Training
Biomechanical Mechanisms Analysis
When standing on one leg, the human balance system initiates a three-level compensation mechanism: first, micro-adjustments at the ankle joint; second, hip joint swinging; finally, compensatory movements of the upper limbs. Research from the Royal Physiotherapy Association in the UK shows that cumulative daily single-leg training of 15 minutes can increase dynamic balance indices by 42% after six weeks.
Safe Training Progression Pathway
A three-level support system is recommended: initially hold a fixed chair back → in the intermediate stage, hold an activity chair back → in the later stage, practice without support. As the training progresses, placing a memory foam pad beneath the standing leg can enhance training intensity through an unstable surface. It is advisable to do this 3-4 times per week, with each session lasting until slight tremors occur, which is optimal for muscle fiber recruitment.
Cross-Dimensional Health Benefits
In addition to improving balance, this training has a significant beneficial effect on knee joint stability. The Tokyo Institute of Gerontology in Japan found that sustained practitioners had an average increase of 0.3 in bone mineral density T scores, which is important for preventing osteoporotic fractures. It is recommended to combine this with breathing exercises, inhaling while rising onto the toes and exhaling while slowly lowering, creating a dual stimulus for neuromuscular activation.
3. Lateral Leg Raise Strength Training
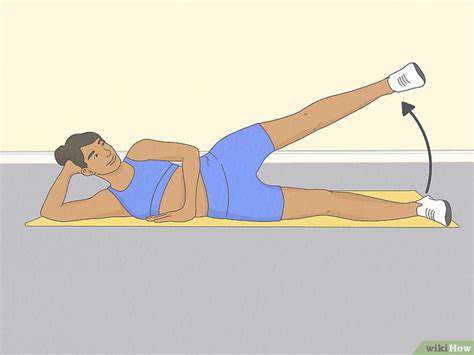
Training Value from an Anatomical Perspective
This movement mainly strengthens the gluteus medius and tensor fasciae latae, both of which are crucial for maintaining pelvic stability during the gait cycle. Clinical data shows that for every 10% increase in hip abductor muscle strength, the risk of falling decreases by 7%. When training, care should be taken to maintain a neutral position of the torso, avoiding compensatory lateral tilting.
Key Points for Controlling Motion Variables
- In the initial stage, a 30-degree leg raise angle is advisable.
- The motion rate should be controlled at 4 seconds for raising and 4 seconds for lowering.
- The feet should remain in a dorsiflexed position to activate the tibialis anterior muscle group.
Advanced practitioners can try tying a 0.5-1 kg sandbag around the ankle or switch to lateral leg raises while lying supine. It is worth noting that after training, the iliotibial band should be relaxed, and using a foam roller for 3 minutes of myofascial release is recommended.
4. Chair Stand Training
Functional Strength Development Program
This training focuses on strengthening the quadriceps and gluteus maximus, which together account for 60% of the total lower limb muscle mass. It is advisable to use an eccentric-concentric combination mode: 3 seconds of slow sitting → 1 second of quick standing up. Research shows that this training method can improve muscle explosive power by 29% compared to traditional methods.
Environmental Adaptation and Risk Management
The height of the chair should allow for a knee flexion of 100-110 degrees; chairs that are too hard or too soft can affect the force exertion pattern. For those with more conspicuous joint degeneration, assistive straps can be installed on both sides of the chair to help relieve the knee joint load with the upper limbs. It is advisable to limit training frequency to 4 times a week to avoid overuse injuries.
5. Balance Beam Walking Training
Neuroplasticity Training Mechanism
Walking on a narrow base compels the cerebellum to continuously make postural adjustments, and this adaptive change can enhance the integration capacity of the vestibular-visual-proprioceptive system. Research published in the German Journal of Sports Medicine indicates that training on a balance beam for 10 minutes, three times a week, can improve dynamic balance scores by 51% after three months.
Innovations in Multidimensional Training
It is recommended to incorporate cognitive training to increase difficulty, such as performing simple calculations or naming objects while walking. This dual-task training mode better simulates real-life scenarios, enhancing the ability to cope with sudden changes. Adjustable-width balance boards can be used, gradually reducing the width from 15 cm to 5 cm for progressive training.
6. Tai Chi Health Practices
Modern Interpretation of Traditional Practices
Tai Chi training activates deep fascial chains through spiral movement trajectories, and its unique center of gravity transfer mode can significantly improve postural control ability. A study by Hong Kong Polytechnic University found that practicing the 24-form Tai Chi three times a week for 12 weeks can enhance lower limb proprioceptive sensitivity by 37%.
Action Decomposition Teaching Strategies
A four-stage learning method is recommended: practice cloud hands decomposition → specific training for center of gravity transfer → rhythm control of breathing → linking the full routine. For those with coordination issues, chair Tai Chi training can be carried out first, gradually transitioning to standing practice. It is important to choose practice areas with good air circulation and avoid training on an empty or overly full stomach.
7. Advanced Applications of Tai Chi Practices
Energy Metabolism Characteristic Analysis
The energy expenditure during Tai Chi practice is equivalent to 2.5 METs, categorized as moderate-intensity aerobic exercise. Its unique abdominal breathing technique can increase tidal volume by 40%, effectively improving cardiovascular and pulmonary function. It is advised to drink 200ml of warm water before morning practice and engage in 10 minutes of meditation post-training to consolidate the training effects.
Building a Social Support System
Participating in community Tai Chi groups not only provides professional guidance but is also vital for establishing a sports social network. Research from the American Geriatrics Society confirms that group practice adherence is 63% higher than solo practice. It is suggested to choose a coach with a lively teaching style and appropriately integrate musical elements to enhance training enjoyment.