Improve Stability with These Senior Friendly Balance Moves
List of Contents
- Older adults generally face issues with deteriorating balance, significantly increasing the risk of falls
- Strength training and other physical activities can effectively improve the exercise capacity of the elderly
- Self-assessment tools help elderly individuals accurately perceive their own balance levels
- Personalized balance training programs consider both safety and exercise effectiveness
- Psychological factors affecting exercise capacity are often overlooked
- Professional guidance enhances training scientificity and reduces the risk of exercise injuries
- Home environment modifications facilitate daily balance training
- Progressive training models ensure continuous improvement
- Scientific monitoring ensures training safety and effectiveness
- Recovery management is crucial for muscle repair
- Key points for selecting age-appropriate exercise equipment
- The key roles of warm-up exercises are analyzed
- Training techniques integrated into daily life scenarios
- The importance of teamwork in medical care
1. The Importance of Maintaining Balance in Older Adults
1. Potential Risks of Balance Deterioration
As age increases, the musculoskeletal and nervous systems of older adults gradually deteriorate, which naturally affects their balance abilities. Statistics show that about one-third of older adults accidentally fall each year due to balance disorders, with hip fractures and head injuries being the most common severe consequences. These accidents not only affect the quality of life but may also lead to complications from long-term bed rest.
Clinical observations have found that declines in lower limb muscle strength, reduced joint mobility, and impaired proprioception are the three main causes of imbalance. This complex degeneration often accelerates rapidly in a short period, emphasizing the importance of early identification of warning signs. For example, an increased frequency of wall-supported walking or swaying when getting up at night are signals to be vigilant about.
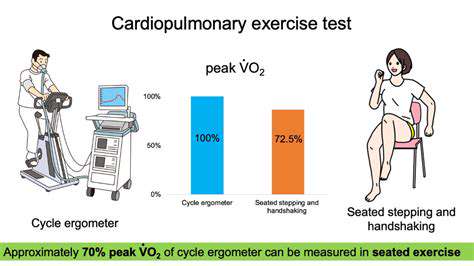
2. The Role of Physical Activity in Improving Exercise Capacity
Regular exercise has been proven to be the best way to maintain the exercise capacity of older adults. Specific training to enhance lower limb muscle strength, combined with flexibility exercises, can significantly improve gait stability. Follow-up surveys by the American College of Sports Medicine show that six months of strength training can reduce the risk of falling by 42%.
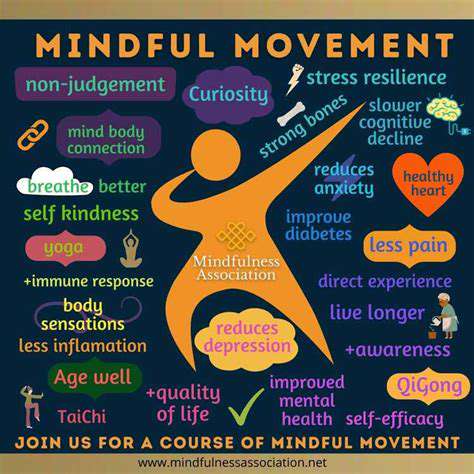
Exercises like Tai Chi, which emphasize center control, are particularly suitable for older adults. Its slow, smooth movements can both train deep muscle groups and enhance spatial awareness. Research from Boston University indicates that Tai Chi training three times a week for 40 minutes each session resulted in an average 37% improvement in balance test scores after three months.
Group exercise projects also have a social incentives effect. Older adults are more likely to maintain enthusiasm for exercise in group training, which is crucial for long-term adherence due to this positive psychological suggestion.
3. Practical Applications of Self-Assessment Tools
Accurately assessing current balance levels is a necessary step before formulating a training plan. The Berg Balance Scale used by medical institutions contains 14 daily action test items that can systematically assess static and dynamic balance abilities. Families can use a simplified version for self-testing: standing on one leg with eyes open for less than 12 seconds or taking more than 13 seconds to rise from a chair indicates the need for intervention.
It is recommended to conduct functional tests in slippery areas such as bathrooms, simulating actions like turning to retrieve items. This situational assessment better reflects real-life conditions, helping to formulate targeted improvement plans.
4. Key Points for Designing Personalized Training Programs
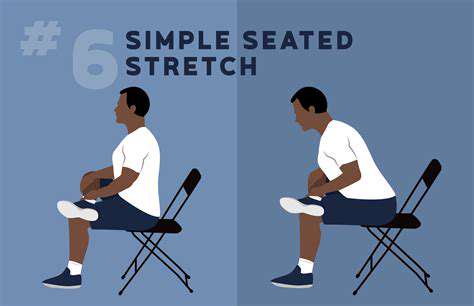
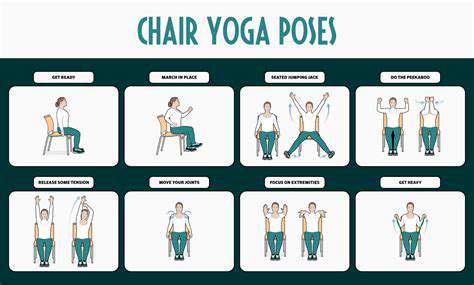
Designing stepwise training programs based on individual differences yields the best results. Initially, one can start with seated balance training, gradually transitioning to chair-supported standing exercises. When single-leg standing can be maintained for over 30 seconds, one can attempt closed-eye training or introduce unstable surfaces (e.g., balance pads).
The tree pose in yoga significantly activates core muscle groups. It is suggested to practice initially with the back against a wall, stabilizing with hands on the back of a chair. As abilities improve, one can attempt to abduct the knee of the raised leg, further challenging balance limits.
Care should be taken to maintain an adaptation period of 2-4 weeks at each advancement stage. Real-time guidance from professional coaches can promptly correct erroneous postures and avoid compensatory injuries.
5. The Influence of Psychological Factors on Exercise Performance
The fear of falling is prevalent among older adults and can lead to a significant decrease in activity, creating a vicious cycle. Research published in the Canadian Journal of Geriatric Medicine indicates that psychological interventions combined with physical therapy can enhance rehabilitation outcomes by 58%.
Support and encouragement from family members can effectively alleviate exercise anxiety. It is recommended to have family members supervise during initial training, providing verbal encouragement to help build confidence. Positive feedback reinforcing a sense of achievement should be given promptly after completing challenging movements.
6. The Value of Support from Professional Medical Teams
Rehabilitation therapists can formulate precise training plans based on examination reports. For example, for patients with osteoporosis, low-impact seated training is prioritized, while those with arthritis would focus on improving joint mobility. Regular follow-ups can dynamically adjust training intensity, ensuring that individuals remain on a safe and effective improvement trajectory.
It is suggested to conduct a comprehensive physical fitness assessment quarterly, with a focus on monitoring gait parameters and reaction speed. This systematic tracking can promptly identify potential risks and avoid the accumulation of exercise injuries.
2. Practical Home Balance Training Plans
The Core Value of Balance Training for Elderly Health
Improving balance ability is not only necessary for fall prevention but also the foundation for maintaining independent living skills. The World Health Organization reports indicate that older adults with good balance ability have an average extension of 7.2 years in their ability to perform daily self-care. This ability directly affects the quality of execution for basic life skills such as shopping and cooking.
From a physiological mechanism standpoint, balance training can simultaneously improve three major systems: vestibular function, visual positioning, and proprioception. The Japan Geriatrics Society recommends 20 minutes of targeted training daily, which has a significant effect on delaying neurodegenerative changes.
Explanation of Classic Home Training Movements
1. Heel-to-toe walk: Choose a straight path of about 3 meters and keep your heel and toe in zero distance contact. This movement can strengthen ankle stability, recommended to practice daily in 3 sets of 10 steps each.
2. Stair balance training: Use stairs for center-of-gravity transfer exercises. With one hand holding the railing, slowly shift your weight to the front of your foot, maintaining for 5 seconds before returning. This movement is particularly suited for improving balance control when going up and down stairs.
Home Environment Modification Tips
Smart use of existing furniture can enhance training safety: use the dining table as a support platform for lunge exercises, or place a yoga mat next to the sofa for floor training. Door frames can serve as vertical reference points to help correct body posture, and tile joints can act as natural balance pathway markers.
It is advisable to set up auxiliary handrails in commonly used pathways (like from the bedroom to the bathroom). This environmental modification not only ensures training safety but also facilitates the natural integration of balance practice into daily life.
Training Records and Safety Monitoring
When establishing a training log, key points to record include: duration of single-leg standing, subjective fatigue levels upon completing sets, and any abnormal bodily responses. Use wearable devices to monitor heart rate changes, ensuring that exercise intensity is kept within 50-70% of the maximum heart rate range. Should dizziness or joint pain occur, training should be halted immediately and rehabilitation physicians consulted.
3. Strategies for Integrating Balance Training into Daily Life

The Core Principles of Life-Based Training
Integrating balance training into daily activities can significantly enhance adherence. For example, doing calf raises while brushing teeth or practicing weight shifts while waiting for a bus. Research from the Royal College of Physiotherapists in the UK confirms that the effectiveness of situational training is 1.7 times that of purely gym-based training.
Kitchen scenario training: When preparing ingredients, perform single-leg standing while cutting vegetables, which can both train balance and improve cooking efficiency. Initially, it is recommended to use a non-slip mat and keep one hand on the counter, gradually transitioning to complete independent standing.
Community Resource Integration Plans
- Utilize park fitness paths for curved walking training
- Join community dance classes to improve rhythmic balance
- Use shopping carts for assisted walking practice while grocery shopping
During public transport, dynamic balance training can be carried out: try to reduce reliance on handrails while the vehicle is in motion, adjusting weight slightly to maintain upright position. This passive training can effectively enhance emergency response abilities.
Application of Digital Assistance Tools
The fall detection feature of smartwatches provides security for seniors living alone. It is recommended to use a fitness app with vibration alert functions, which will issue warnings when body posture deviates from the centerline. Virtual reality balance training systems can simulate various complex scenarios to enhance adaptability in a safe environment.
4. Safety Training Operational Specifications
Guidelines for Selecting Exercise Equipment
When selecting footwear, it is essential to focus on: sole tread depth ≥3mm, moderate hardness of the heel cup, and reasonable degree of forefoot bending. Professional balance training shoes are typically designed with lateral support to effectively prevent ankle inversion. Regarding protective gear, knee straps and waist supports may be used as needed, but excessive reliance should be avoided.
Key Points for Environmental Safety Assessment
The training area should ensure: brightness ≥300 lumens, a floor friction coefficient >0.5, and no sharp furniture within 2 meters. It is recommended to install night lights in main activity areas, using tiles with non-slip grades above R10. During winter training, keep the room temperature at 20-24℃, as low temperatures can decrease muscle response speed.
Progressive Training Cycle Planning
A 3-3-3 progressive model is recommended: each difficulty level lasts for 3 weeks, with training three times a week, and each session includes 3 new movements. For example, the first phase focuses on seated training, the second phase transitions to chair-supported exercises, and the third phase attempts brief independent standing without assistance. Increments at each phase should be controlled within 15-20% for safety.
Fatigue Recognition and Recovery Management
If muscle soreness persists for more than 48 hours post-exercise, or if resting heart rate increases by 10 beats per minute compared to usual, it signifies the need to adjust the training plan. It is recommended to use heat therapy combined with low-frequency pulse therapy to expedite recovery; supplementing with branched-chain amino acids can effectively alleviate delayed soreness. The Japanese Society of Sports Medicine advises that training intervals for those aged 65 and older should ensure at least 48 hours.
Multidisciplinary Collaboration Mechanism
Establish a health management team comprised of primary care physicians, nutritionists, and physical therapists. Regular assessments of bone density and gait analysis should be conducted to adjust dietary calcium intake and training programs based on the examination results. For those on antihypertensives, special attention should be given to the timing of training sessions, avoiding high-intensity exercises during peak drug effect periods.