Staying Strong with Osteoporosis: Exercise Guidelines
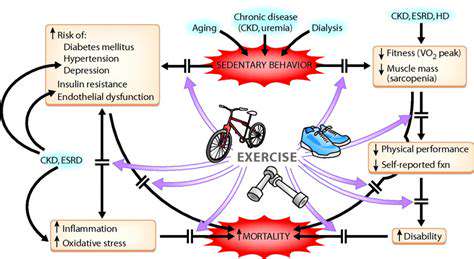
Physical activity serves as a cornerstone in warding off osteoporosis, a condition marked by brittle bones. When we move our bodies consistently, we trigger bone remodeling processes that enhance density and fracture resistance. This proves especially vital during youth when bones develop their peak mass. Later in life, maintaining regular movement helps counteract age-related bone deterioration.
Selection of appropriate activities makes all the difference. Weight-bearing movements - including walking, dancing, and stair climbing - create beneficial stress on bones. These gravity-defying actions stimulate osteoblasts (bone-forming cells) to reinforce skeletal structure. Resistance training with bands or weights offers complementary benefits by fortifying the muscles that support our bony framework.
Tailoring Exercise to Your Needs and Abilities
Personalization remains key when designing an effective bone-health regimen. Consultation with medical professionals ensures safety, particularly for those with pre-existing conditions. They can recommend suitable intensity levels and exercise modalities based on individual capabilities. Beginners should start gently, perhaps with brief sessions of low-impact activity, then progressively challenge themselves as fitness improves.
The body provides valuable feedback during this process. Discomfort signals the need to scale back, while improved endurance indicates readiness for greater challenges. Early focus should center on establishing consistent habits rather than pushing intensity boundaries.
Beyond Weight-Bearing: The Role of Other Exercises
While bone-loading activities take center stage, other movement forms contribute valuable supporting roles. Aquatic exercises and cycling, though non-weight-bearing, maintain cardiovascular health and preserve muscle mass - both critical for skeletal support. These activities prove especially valuable for those needing joint-sparing options.
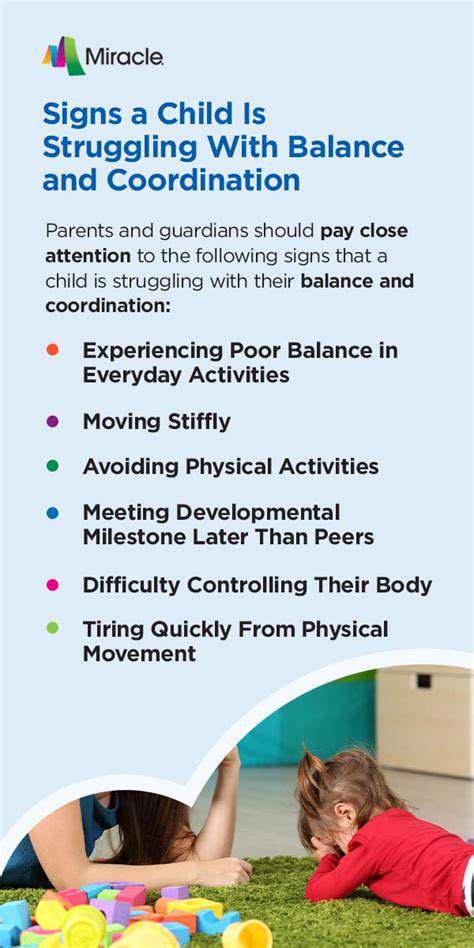
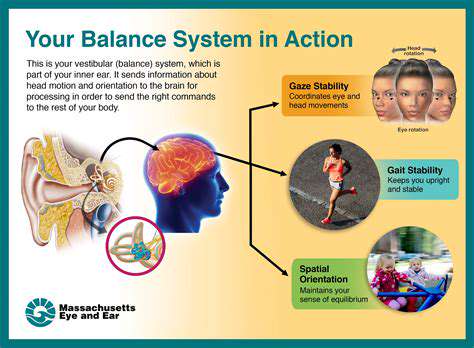
Balance-focused practices like tai chi offer fracture prevention through improved stability. By enhancing proprioception (body awareness in space), these disciplines reduce fall likelihood - a major concern for osteoporotic individuals.
The Importance of Exercise Duration and Frequency
Regularity transforms exercise from sporadic effort to bone-protecting lifestyle. Aim for 30-minute sessions of weight-bearing activity most days, supplemented by resistance training 2-3 weekly. Sustainable routines prove more effective than intermittent intense workouts. The cumulative effect of persistent, moderate effort yields the greatest bone-preserving benefits.
Nutrition and Exercise: A Powerful Combination
Movement alone doesn't complete the bone-health equation. Dietary support through calcium-rich foods and vitamin D sources enables exercise's bone-building effects. These nutrients work synergistically - calcium provides structural material while vitamin D ensures its proper utilization. Professional nutritional guidance can optimize this combination for individual needs.
When consistent physical activity pairs with targeted nutrition, the body receives comprehensive support for maintaining skeletal integrity throughout life's stages.

Safe Exercise Practices for Individuals with Osteoporosis
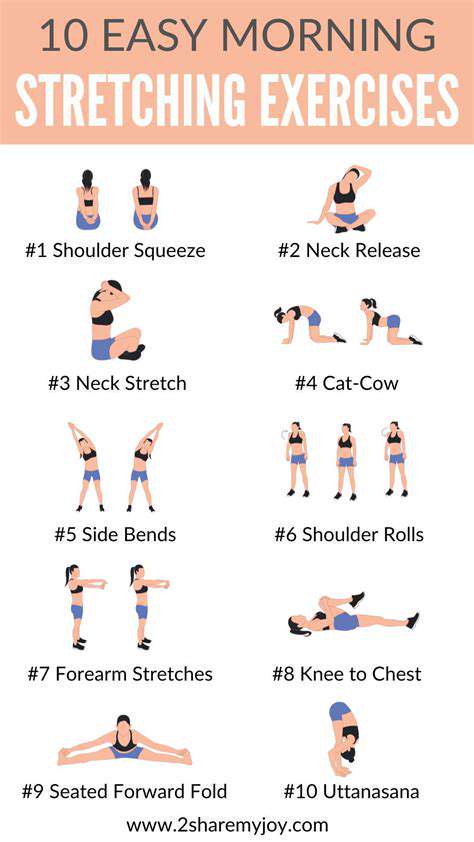
Warm-up and Cool-down Routines
Proper preparation protects vulnerable bones before activity. Gradual warm-ups increase circulation and joint lubrication, while cool-downs facilitate recovery. This two-phase approach proves particularly valuable for fragile skeletal systems. Simple movements like arm circles prepare the upper body, while gentle marches ready the lower extremities.
Dynamic stretches (moving through ranges of motion) optimally prepare the body for action. Post-activity, static stretching held for 15-30 seconds helps maintain flexibility. Always honor the body's signals - persistent discomfort warrants immediate cessation and professional consultation.
Choosing Appropriate Exercises
Activity selection requires careful consideration of bone health status. Weight-bearing options should dominate, with resistance work providing complementary strength. Low-impact variations often suit osteoporotic individuals better than their high-impact counterparts. Aquatic activities offer excellent alternatives when land-based exercise proves challenging.
Medical professionals can assess bone density and recommend appropriate modifications. Their guidance helps navigate the balance between sufficient challenge for bone stimulation and excessive risk of fracture.
Proper Form and Technique
Movement quality outweighs quantity when bones are vulnerable. Precise alignment distributes forces evenly across joints and bones. During resistance exercises, core engagement protects the spine, while controlled motions prevent harmful torque. Those uncertain about proper mechanics should seek qualified instruction to establish safe movement patterns.
Listening to Your Body and Rest
Attentiveness to physical signals prevents overuse injuries. Rest days allow for bone remodeling and tissue repair - essential processes often overlooked. Discomfort during activity should never be ignored, as it may indicate excessive skeletal stress. Periodic professional reassessment ensures continued exercise appropriateness as bone health evolves.
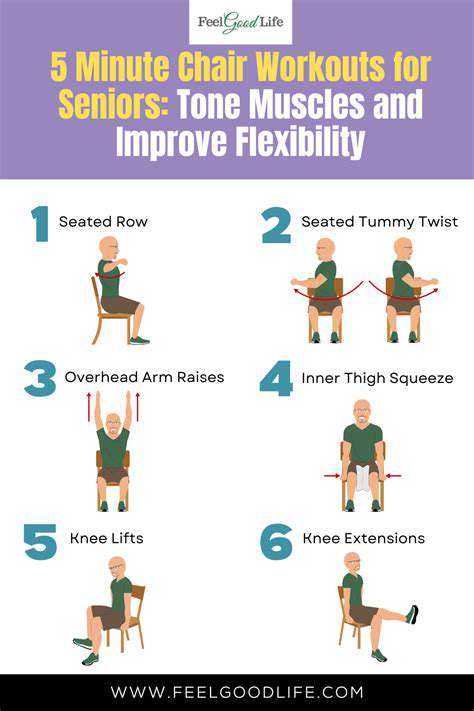
Modifying Exercises for Osteoporosis
Adaptation transforms potentially risky movements into safe, effective options. Reduced range versions, supported positions, or equipment substitutions can make activities accessible. For instance, wall push-ups replace floor versions, while seated rows substitute for standing variations. Professional guidance helps identify optimal modifications for individual circumstances.
Nutrition and Lifestyle Considerations

Nutritional Strategies for Optimal Health
Whole food consumption forms the foundation of skeletal support. Vibrant produce provides bone-friendly nutrients beyond just calcium and vitamin D. Magnesium from leafy greens and omega-3s from fatty fish contribute to bone matrix formation. Processed food limitation reduces inflammatory compounds that may interfere with bone metabolism.
Hydration: The Unsung Hero
Adequate fluid intake maintains the cushioning properties of intervertebral discs and joint spaces. Water comprises a significant portion of bone composition, making hydration a direct contributor to skeletal health. Herbal infusions and mineral waters offer flavorful alternatives to plain water while contributing beneficial compounds.
Mindful Eating Practices
Conscious consumption enhances nutrient absorption and satisfaction. Slowing meal pace allows better recognition of satiety signals, preventing overconsumption that stresses the skeletal system. This practice also improves digestion, ensuring optimal extraction of bone-supporting nutrients from foods.
Lifestyle Factors Influencing Nutrition
Regular movement enhances nutrient utilization while sedentary habits impair metabolic efficiency. Weight-bearing activity not only stimulates bones directly but also improves circulation of bone-building nutrients. Outdoor exercise offers the dual benefit of movement and vitamin D synthesis when performed in sunlight.
Stress Management Techniques
Chronic tension elevates cortisol, which can accelerate bone loss over time. Relaxation practices counteract this effect by modulating stress hormone production. Breath-focused methods prove particularly accessible, requiring no special equipment while offering immediate calming effects.
Sleep Hygiene and its Impact
Nocturnal restoration facilitates bone remodeling processes. Deep sleep stages coincide with peak growth hormone release, crucial for tissue repair including bone. Consistent sleep schedules align with circadian rhythms that regulate bone metabolism hormones. A dark, cool sleeping environment optimizes these natural processes.