Chair Yoga for Seniors with Multiple Sclerosis: Adapting Your Practice
Diaphragmatic breathing, sometimes called belly breathing, forms the cornerstone of effective relaxation methods. This approach activates the diaphragm, our main breathing muscle, to fully oxygenate the lungs. Many healthcare professionals recommend this method because it delivers measurable stress reduction benefits. When performed correctly, diaphragmatic breathing enhances oxygen absorption, directly boosting vitality and alertness. Clinical studies show this breathing pattern helps stabilize cardiovascular function, creating profound physiological calm.
For optimal results, position yourself comfortably either seated or supine. Place one palm on your sternum and the other below your ribcage. Inhale deliberately through your nose, feeling your abdomen expand outward. Visualize air filling your lungs completely, from base to apex. Exhale through pursed lips, noticing your belly gently contracting. Regular practice yields cumulative benefits - most practitioners report better sleep quality and emotional regulation within weeks. This technique works particularly well when combined with gentle stretching.
Mindful Breathing Exercises for Stress Reduction
Conscious breathing practices offer powerful antidotes to modern stress. These methods train attention to the subtle sensations accompanying each breath cycle. By anchoring awareness in the present moment, practitioners develop the ability to disengage from repetitive worrying patterns. Neuroscience research confirms these exercises activate the parasympathetic nervous system, our body's natural relaxation response.
Try this basic mindfulness exercise: Focus on the temperature difference between inhaled and exhaled air. Notice how your ribcage expands three-dimensionally with each breath. When distractions arise (as they inevitably will), simply acknowledge them and return focus to your breathing rhythm. Clinical trials demonstrate that just 10 minutes of daily mindful breathing can lower cortisol levels by up to 25%. Many therapists recommend keeping a breathing log to track progress and identify optimal practice times.
Progressive Relaxation Breathing Techniques
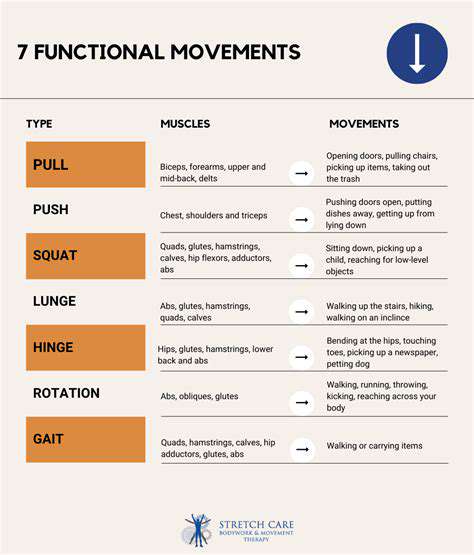
Systematic tension-release methods provide targeted relief for muscle stiffness and nervous tension. These exercises combine breath awareness with deliberate muscle engagement, creating profound mind-body integration. Physical therapists often prescribe these techniques for patients recovering from injuries or managing chronic pain conditions.
Begin by establishing smooth, even breathing. Then sequentially contract muscle groups - start with your dominant hand, making a tight fist while inhaling. Hold briefly, then release completely during exhalation. Progress through major muscle groups, paying special attention to areas holding habitual tension. This method proves particularly effective when practiced before bedtime, as it prepares both body and mind for restorative sleep. For enhanced benefits, combine with aromatherapy using lavender or chamomile essential oils.
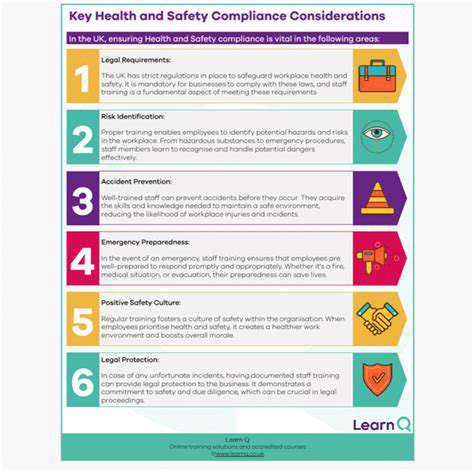
Safety Precautions and Considerations
Pre-Yoga Assessment
Medical clearance forms the essential first step before initiating any therapeutic movement program. A qualified healthcare provider can evaluate how MS symptoms might affect your practice. This evaluation should include discussion of current medications, as some prescriptions may influence balance or fatigue levels. Many rehabilitation specialists recommend starting with video-recorded sessions to monitor form and progress safely.
Keep a symptom journal noting any changes in mobility, sensation, or energy levels. This documentation helps tailor future sessions to your evolving needs while identifying potentially problematic movements early.
Proper Posture and Support
Optimal seating setup dramatically enhances practice safety and effectiveness. Select a chair with firm cushioning and adequate back support - many physical therapists recommend wooden kitchen chairs over plush armchairs for better stability. Proper spinal alignment reduces unnecessary muscular effort, allowing fuller focus on breath and movement quality. For those with postural challenges, rolled towels can provide customized lumbar support.
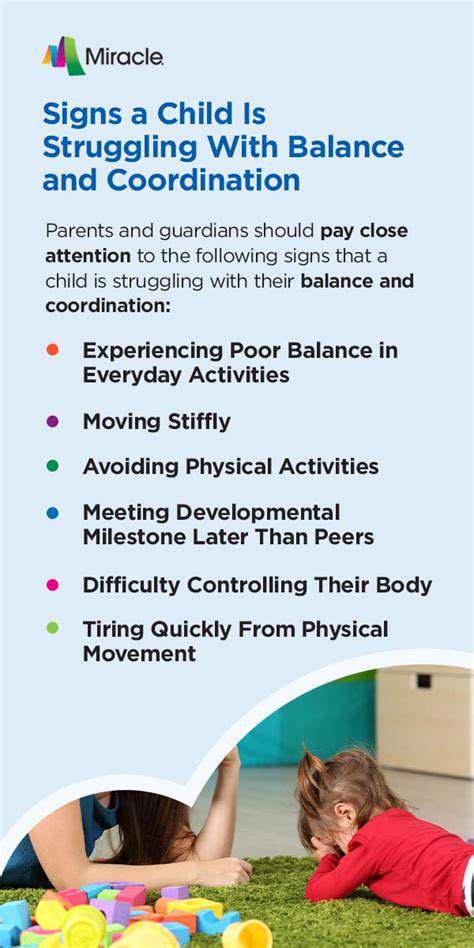
Feet should maintain full contact with the floor; if needed, use yoga blocks or phone books underfoot to achieve proper knee alignment. This grounded position enhances proprioceptive feedback, crucial for maintaining balance during transitions.
Modifications and Adaptations
Therapeutic yoga emphasizes intelligent adaptation over rigid form. If standard poses prove challenging, explore variations using household items - a belt can extend reach, while pillows can reduce joint strain. Many instructors recommend the 50% rule - only working within half your perceived capacity to prevent overexertion. This conservative approach allows gradual strength building without triggering symptom flare-ups.
For example, when performing seated twists, keep movements small and controlled. Use chair arms for leverage rather than forcing rotation. These thoughtful modifications make the practice accessible while still delivering therapeutic benefits.
Breathing Techniques
Conscious respiration serves as the bridge between physical movement and neurological benefits. MS specialists often teach triangle breathing - equal duration inhalation, retention, and exhalation - to regulate autonomic function. This method shows particular promise for managing temperature sensitivity episodes common in MS.
Try synchronizing breath with movement: inhale during extensions, exhale during flexions. This coordination enhances motor control while preventing breath-holding, which can spike blood pressure. Research indicates regular breathing practice can improve bladder control and reduce spasticity in MS patients.
Hydration and Nutrition
Optimal fluid intake proves especially critical for neurological conditions. Begin hydrating at least two hours before practice, aiming for pale yellow urine as an indicator. Many nutritionists recommend electrolyte-enhanced waters for better cellular hydration. Time meals carefully - a light snack 90 minutes beforehand prevents energy crashes without causing digestive discomfort.
Post-session, replenish with magnesium-rich foods like bananas or almonds to prevent muscle cramps. Some practitioners find tart cherry juice helps reduce post-exercise inflammation.
Listening to Your Body
Develop sensitivity to subtle physiological signals. Notice the difference between productive discomfort (mild muscle engagement) and warning signs (sharp pains or numbness). Keep sessions brief initially - even 10 minutes provides benefits without overtaxing the system. Many therapists recommend the two-hour rule - if symptoms worsen significantly within two hours post-practice, scale back intensity next session.
Track energy fluctuations throughout your menstrual cycle if applicable, as hormone changes often affect MS symptoms. This awareness allows for natural practice adjustments.
Safety Equipment and Considerations
Invest in proper yoga props - non-slip mats under chairs prevent dangerous sliding. Wall-mounted bars offer stability for standing transitions. Consider fingerless gloves for better grip if hand weakness exists. Proper equipment transforms potential hazards into opportunities for progressive challenge.
Always practice near stable support - position your chair near a wall or heavy furniture. Keep emergency contacts and medications easily accessible during sessions. These precautions create psychological safety, allowing fuller immersion in the practice.