Safe Strength Exercises to Build Bone Density in Seniors
Strength Training for Bone Health
Resistance exercise delivers unique benefits for skeletal health. When muscles pull against bones during strength training, they create mechanical stress that triggers bone remodeling. Elastic bands, light dumbbells, or even bodyweight exercises all qualify as effective tools. The key lies in progressive overload—gradually increasing resistance to continue stimulating bone adaptation. This approach works regardless of starting fitness level.
Nutrition and Bone Density
Diet plays a synergistic role with exercise in bone maintenance. Beyond the well-known calcium-vitamin D duo, emerging research highlights the importance of protein, magnesium, and vitamin K. Dairy products certainly help, but so do sardines, almonds, and fermented foods. A surprising fact: the gut microbiome influences calcium absorption, meaning probiotic foods may indirectly support bone health.
Importance of Fall Prevention
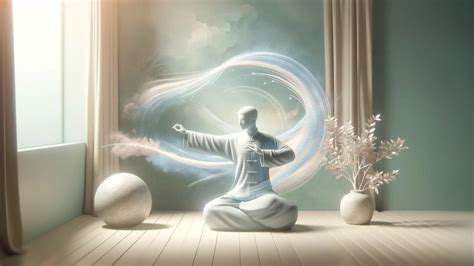
While building stronger bones is crucial, avoiding traumatic impacts matters equally. Balance training should become as routine as brushing teeth for older adults. Simple practices like single-leg stands (near support) or tai chi movements significantly reduce fall risk. Home modifications—removing throw rugs, improving lighting—create safer environments. Remember: preventing one hip fracture can add years of active independence.
Consulting Healthcare Professionals
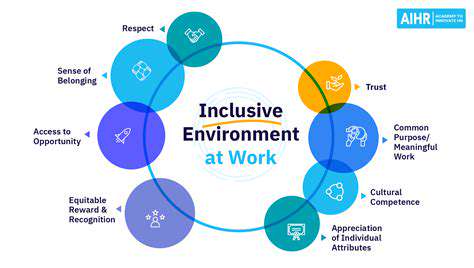
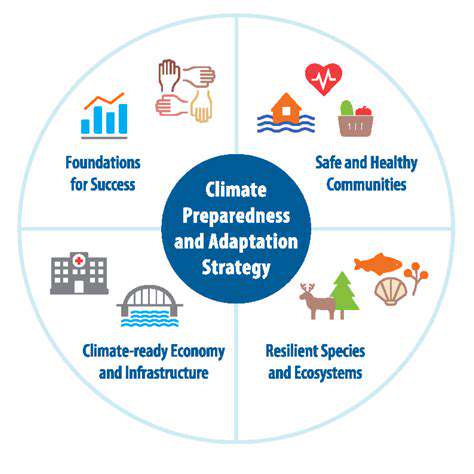
Personalized guidance makes all the difference. Geriatricians can assess fracture risk through bone density scans, while physical therapists design targeted exercise regimens. Nutritionists identify dietary gaps, and pharmacists review medications that might affect bone metabolism. This multidisciplinary approach addresses bone health from all angles, creating comprehensive protection.
Weight Training for Seniors: A Cautious Approach
Understanding the Benefits of Weight Training for Seniors
Resistance training offers seniors benefits far beyond muscle growth. Studies demonstrate it can improve neural activation patterns, essentially waking up dormant muscle fibers. This translates to better movement control and reaction times—critical for fall prevention. The psychological benefits are equally impressive, with many seniors reporting improved confidence in daily activities.
The key lies in appropriate programming. Unlike younger athletes chasing performance gains, older adults should prioritize controlled movements with perfect form. This approach maximizes benefits while minimizing injury risk.
Assessing Your Physical Condition and Needs
Comprehensive pre-exercise screening should evaluate more than just medical history. Functional movement assessments identify compensation patterns that could lead to injury. Gait analysis reveals balance deficits, while grip strength testing serves as a surprising predictor of overall health status. These assessments create a baseline for tracking progress beyond simple weight numbers.
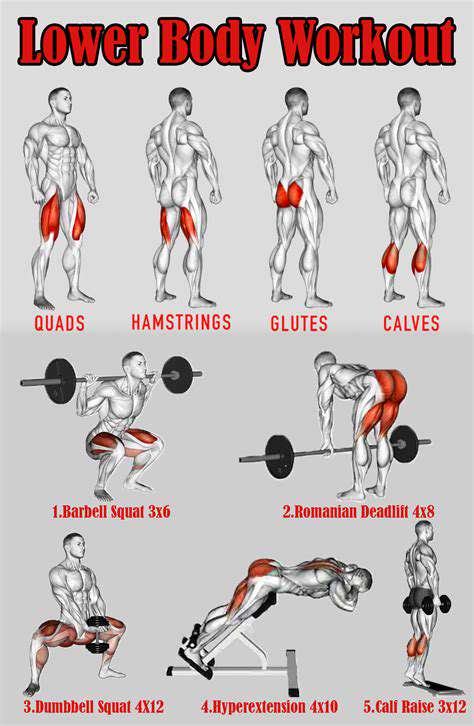
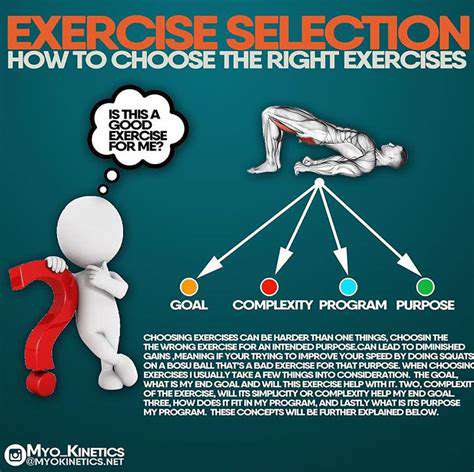
Choosing the Right Exercises and Equipment
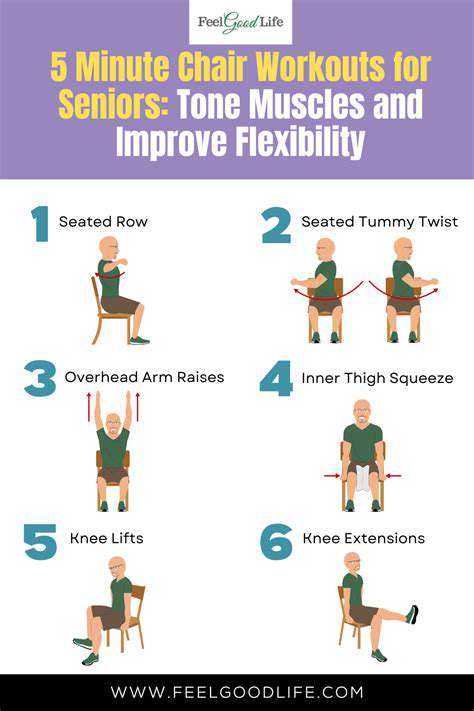
Exercise selection should target functional movement patterns—squatting, pushing, pulling, and carrying. Resistance bands offer excellent versatility, allowing adjustment of resistance through range of motion. For those with arthritis, neoprene-coated dumbbells provide more comfortable grip surfaces. Seated exercises can provide safe alternatives for those with balance concerns.
Gradual Progression and Proper Form
The 10% rule applies well to senior strength training—never increase weight by more than 10% weekly. Focus on tempo control, emphasizing slow eccentric (lowering) phases. Three-second eccentrics not only enhance safety but also increase time under tension for greater strength gains. Mirrors or video feedback help maintain proper alignment.
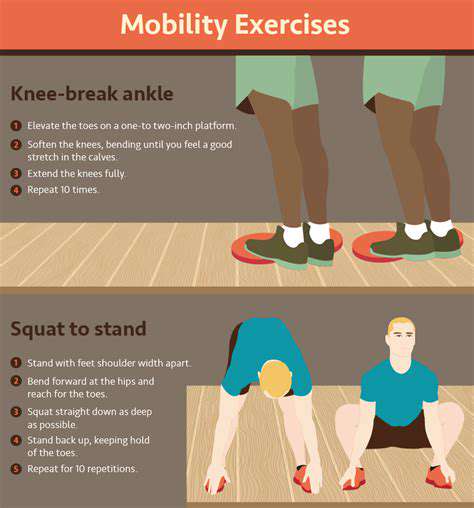
Safety Precautions and Warm-up/Cool-down Routines
Dynamic warm-ups should address the specific movements in the workout. For upper body days, arm circles and band pull-aparts prepare the shoulders. Lower body sessions benefit from hip openers and bodyweight squats. Cool-downs should include static stretching held for 30-60 seconds to maintain flexibility. Always keep water nearby and consider workout timing—morning sessions may suit those with arthritis better.
Consistency and Patience in Building Strength
Neuromuscular adaptations precede visible muscle changes. Most seniors notice improved movement ease within 4-6 weeks, while measurable strength gains typically appear by week 8-12. Tracking non-scale victories—easier grocery carrying, less stair fatigue—provides powerful motivation. Remember, consistency trumps intensity in the long run.
Staying Consistent and Listening to Your Body
Understanding the Importance of Consistency
The body responds best to regular, rhythmic stimulation. For bone density, three 30-minute sessions weekly prove more effective than one marathon session. This frequency maintains consistent mechanical loading that osteocytes (bone cells) respond to. Creating an exercise appointment in one's calendar increases adherence significantly.
Listening to Your Body: Recognizing Pain Signals
Learn to distinguish good pain (muscle fatigue) from bad pain (joint or sharp pain). A useful guideline: discomfort should be symmetrical—if one side hurts significantly more, something's wrong. Morning stiffness lasting less than 30 minutes is generally normal; prolonged stiffness warrants professional evaluation.
Choosing Appropriate Exercises for Bone Health
Multi-planar movements challenge bones most effectively. Instead of just forward lunges, try adding lateral and diagonal variations. Vibration platforms show promise for those with limited mobility—standing on them for 10 minutes daily may stimulate bone growth. Always prioritize weight-bearing positions over seated exercises when possible.
Prioritizing Proper Form and Technique
The talk test helps gauge intensity—you should be able to speak in short phrases during exercise. If you can't talk at all, the effort is too intense; if you can converse easily, you're not working hard enough. For strength exercises, exhale during the exertion phase to maintain core stability.
Gradual Progression and Building Strength
Progress can be measured in multiple dimensions: increased weight, more repetitions, better form, or shorter rest periods. Keeping a simple workout log helps track these subtle improvements over time. Celebrate all progress—even being able to do one more repetition matters.
Importance of Adequate Calcium and Vitamin D Intake
Calcium timing matters—spreading intake throughout the day improves absorption. Vitamin D3 (cholecalciferol) supplements are generally more effective than D2 for raising blood levels. Those taking proton pump inhibitors should be especially vigilant about calcium intake, as these medications can reduce absorption.
Rest and Recovery: Crucial for Bone Health
Bone remodeling primarily occurs during rest. Seven to eight hours of quality sleep allows for optimal bone repair. Contrast therapy (alternating heat and cold) can help manage post-exercise soreness. Active recovery days might include gentle yoga or walking.