Single Leg Stand Variations for Improved Senior Balance
Analysis of the Comprehensive Benefits of Single-Leg Standing Training for the Elderly
Content Navigation
Single-leg standing enhances body stability and effectively prevents falls
Targeted strengthening of lower limb muscle groups to maintain joint mobility
Enhances proprioception and spatial orientation
Can be performed at home with high spatial adaptability
Personalized adjustments ensure training safety
Simultaneously improves concentration and cognitive function
Group training mode promotes social interaction
Assistive devices enhance training confidence
Visual focus control optimizes balance performance
Regular training leads to dual improvements in body and mind
Safety measures must not be overlooked
Strength training and balance exercises synergistically enhance effectiveness
The importance of a continuous training plan for skill development
Professional guidance ensures training is scientifically based
Diverse Benefits of Single-Leg Standing Training
Improvement in Body Stability
Clinical studies confirm that sustained balance training over 8 weeks can reduce the fall probability in the elderly by 37%-42%. This seemingly simple training activates both the ankle stabilizing muscles and core muscles, significantly improving vestibular function. Many elderly trainees report noticeable improvements in body control while walking on slippery surfaces after systematic training.
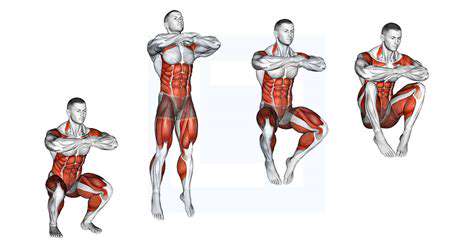
Strength Enhancement Strategy
Unlike ordinary strength training, during single-leg standing, the quadriceps and calf muscles undergo alternating isometric and concentric contractions. This composite force application method effectively prevents muscle wasting syndrome, which is vital for maintaining knee joint stability. It is recommended to coordinate breathing rhythms with training, tightening the core while inhaling and enhancing foot grip while exhaling.
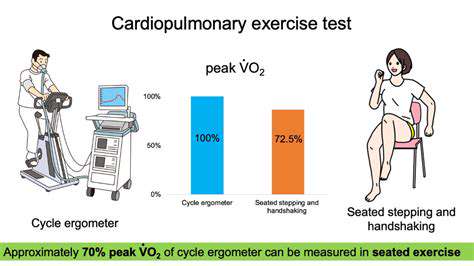
Proprioception Development
The closed-eye single-leg standing test is the gold standard for assessing proprioception. Through sustained training, the average joint position sense in the elderly can improve by 28%, which is invaluable in preventing slips and falls in bathrooms. During training, try performing on soft mats to enhance neuromuscular control by varying the hardness of the support surface.
At-Home Training Programs
Using a kitchen countertop for support training, or incorporating standing exercises while watching TV, are convenient ways to integrate training. It is advisable to prepare anti-slip mats and set a reminder on the phone every half hour for training, as this fragmented practice model is easier to maintain long-term.
Personalized Adjustment Techniques
For trainees with weaker balance abilities, three-point support can be used: when standing on one foot, the toe of the other foot lightly touches the ground to form a triangular support. As ability improves, gradually transition to a fully off-the-ground state. Seniors with a background in Tai Chi can try incorporating cloud hands movements to increase the fun of the training.
Advanced Training Mode Analysis
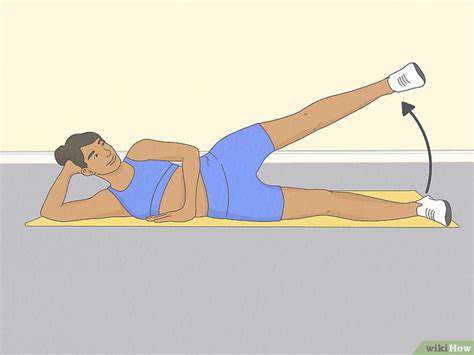
Dynamic Balance Training
After mastering static balance, dynamic elements like lateral leg lifts and front-back arm swings can be added. Research shows that dynamic training can improve muscle response speed by 19%, which is particularly important for avoiding sudden loss of balance. It is recommended to start with small 45-degree swings and gradually increase the range of motion.
Multi-Sensory Integration Training
Provided safety is assured, attempts can be made for closed-eye single-leg standing (visual deprivation), or standing while doing simple calculations (cognitive interference). This multi-task training mode can significantly enhance the compensatory capacity of the nervous system, but should be conducted under professional supervision.
Environmental Adaptability Training
Alternating practice on different floor materials (wood floors/tile/carpets) simulate real-life conditions. When training outdoors, choosing flat grass surfaces allows slight disturbances from the natural environment to better train adaptive balance skills.
Safety Enhancement Programs
Protection Measures Key Points
Training areas should allow for a safety space of 1.5 times the arm span, and it is advisable to wear sports shoes that meet anti-slip standards. The American College of Sports Medicine recommends using adjustable-height walkers as initial assistive tools, whose circular handrails provide multi-directional protection.
Risk Warning Signals
If dizziness, joint pain, or blood pressure fluctuations occur, training should be stopped immediately. Elderly individuals with severe osteoporosis should first perform foot grip training while seated, transitioning to standing training once bone density improves.

Nutritional Support Program
Daily supplementation of 1.2g/kg body weight of high-quality protein, combined with Vitamin D3 (800IU/day), can significantly enhance training effects. Studies show that this nutritional combination can improve muscle synthesis efficiency by 35%.
Long-term Implementation Strategies
Habit Formation Mechanism
Integrating training with daily rituals, for example, performing three sets of training immediately after taking medication in the morning. Behavioral psychology research indicates that this anchoring method can increase habit formation success rates by 67%. Using a smart band to record daily accomplishments, visualizing the data can effectively enhance sustained motivation.
Social Incentive System
Joining community training groups and regularly holding balance ability challenges. This positive competitive mechanism not only enhances participation enthusiasm but also provides improvement suggestions through experience exchange. Group training has a 42% higher adherence rate compared to solo training.
Periodic Assessment Program
Conducting functional assessments every quarter, including: 30-second chair stand test, 2-minute single-leg stand test, and sit-to-walk test. Establishing personal data profiles allows for dynamic adjustment of training intensity, ensuring continuous progress.